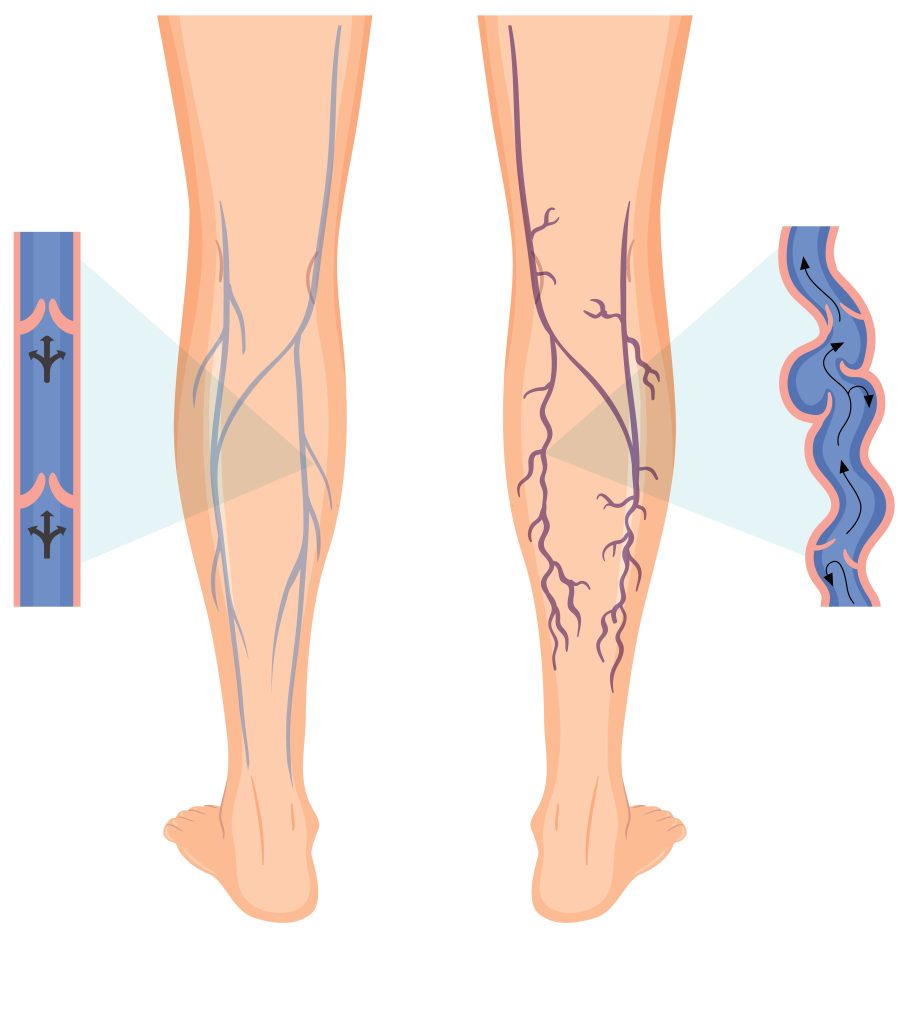
Venous insufficiency is a condition in which the veins, most commonly in the legs, have difficulty returning blood back to the heart. This happens when the valves in the veins become weak or damaged, causing blood to pool in the lower extremities instead of flowing upward. As a result, pressure builds in the veins, leading to symptoms such as leg swelling, pain, heaviness, skin discoloration, and in severe cases, ulcers near the ankles. It is often caused by factors such as varicose veins, deep vein thrombosis, prolonged standing, obesity, or aging. Treatment focuses on improving blood flow, often through lifestyle changes, compression therapy, and in some cases, medical or surgical intervention.
Venous insufficiency causes :
Venous insufficiency is primarily caused by weakened or damaged valves within the veins, which are responsible for keeping blood flowing in one direction—toward the heart. When these valves fail, blood can flow backward and pool in the veins, especially in the legs. Common causes include deep vein thrombosis (a blood clot in a deep vein), varicose veins, and conditions that increase pressure in the veins such as obesity, pregnancy, or prolonged standing or sitting. Aging also contributes, as vein walls and valves naturally weaken over time. Additionally, a family history of venous disease or a sedentary lifestyle can increase the risk of developing venous insufficiency.
- Deep vein thrombosis (DVT)
- Varicose veins
- Obesity
- Pregnancy
- Prolonged standing or sitting
- Age-related weakening of vein walls or valves
- Family history
The symptoms of venous insufficiency :
develop gradually and often worsen over time. Common signs include swelling in the lower legs and ankles, a feeling of heaviness, aching, or cramping in the legs—especially after standing or sitting for long periods. Patients may also notice varicose veins, which appear as twisted, enlarged veins close to the surface of the skin. Skin changes are common, such as itching, dryness, or a reddish-brown discoloration around the ankles. In more advanced cases, the condition can lead to painful venous ulcers, usually near the inner ankles, that are slow to heal. These symptoms tend to improve with leg elevation and worsen with prolonged immobility.
- Leg swelling (edema)
- Aching, cramping, or heaviness in the legs
- Varicose veins
- Skin discoloration (brownish or reddish, especially near the ankles)
- Itchy or scaly skin on the legs
- Venous ulcers (typically around the ankles)
- Worsening symptoms with standing or sitting for long periods

Venous insufficiency focuses solutions :
The treatment of venous insufficiency focuses on improving blood flow, relieving symptoms, and preventing complications. Conservative approaches are often the first step and include wearing compression stockings to support the veins, elevating the legs regularly to reduce swelling, and engaging in physical activity such as walking to promote circulation. Lifestyle changes, such as maintaining a healthy weight and avoiding prolonged periods of standing or sitting, are also important. In more severe cases, medical procedures may be necessary, such as sclerotherapy (injecting a solution into affected veins), endovenous laser or radiofrequency ablation (using heat to close damaged veins), or surgical removal of varicose veins. Proper wound care is essential if venous ulcers are present. With appropriate management, symptoms can be significantly reduced and complications prevented.
Conservative (first-line)
- Compression stockings (improve blood flow and reduce swelling)
- Leg elevation (above heart level when possible)
- Regular exercise (especially walking)
- Weight loss and lifestyle changes
Medical/Surgical
- Sclerotherapy (injection into varicose veins)
- Ablation therapy (radiofrequency or laser to close faulty veins)
- Vein stripping or ligation (removal or tying off damaged veins)
- Angioplasty and stenting (for central vein obstruction)
- Management of venous ulcers (wound care, dressings)
