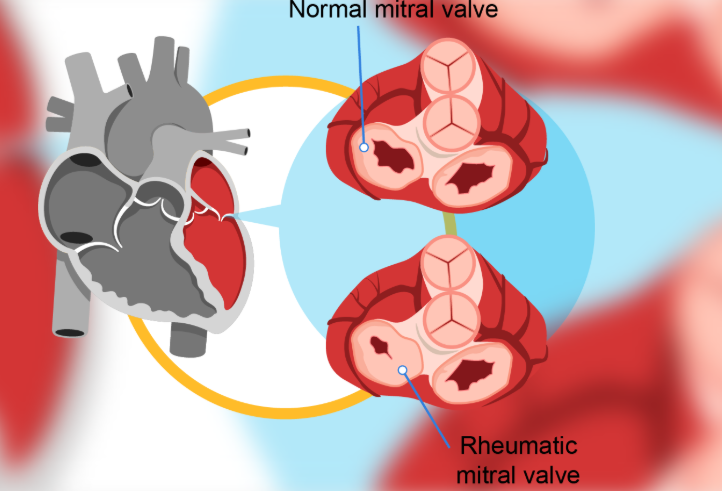
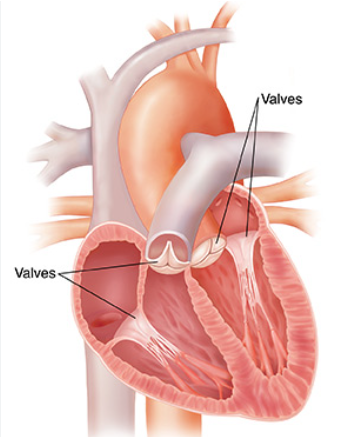
Rheumatic valve disorders are chronic deformities of the cardiac valves (especially mitral and aortic) caused by fibrosis, thickening, and calcification following rheumatic fever, resulting in valvular stenosis, regurgitation, or both.

The causes of rheumatic valve disorders:
1. Primary Cause
- Rheumatic fever → an autoimmune, post-infectious complication of group A β-hemolytic streptococcal (Streptococcus pyogenes) pharyngitis or tonsillitis.
- The body produces antibodies against streptococcal antigens, but due to molecular mimicry, these antibodies cross-react with proteins in the heart valves, myocardium, joints, and skin.
- This autoimmune reaction causes valvulitis → scarring → deformity.
2. Contributing Factors
- Recurrent or untreated strep throat infections (especially in childhood).
- Low socioeconomic conditions (overcrowding, poor access to healthcare).
- Lack of antibiotic treatment for streptococcal infections.
- Genetic susceptibility (some individuals mount a stronger autoimmune response).
Types of Rheumatic valve disorders:
Rheumatic valve disorders primarily affect the mitral and aortic valves, though other valves can rarely be involved. They can cause stenosis, regurgitation, or a combination.The main types are:
1. Mitral Valve Disorders (Most Common)
- Mitral Stenosis (MS):
- Narrowing of the mitral valve orifice due to leaflet thickening, commissural fusion, and chordae shortening.
- Leads to left atrial enlargement, pulmonary congestion, and atrial fibrillation.
- Mitral Regurgitation (MR):
- Incomplete closure of the mitral valve, causing backflow of blood into the left atrium during systole.
- Mixed Mitral Valve Disease:
- Both stenosis and regurgitation features present.
2. Aortic Valve Disorders
- Aortic Stenosis (AS):
- Narrowing of the aortic valve due to leaflet thickening and fusion.
- Causes left ventricular hypertrophy and outflow obstruction.
- Aortic Regurgitation (AR):
- Incomplete closure of the aortic valve, leading to backflow into the left ventricle during diastole.
3. Tricuspid and Pulmonic Valve Involvement (Rare)
- Usually occurs in severe or longstanding rheumatic heart disease.
- Can cause tricuspid regurgitation or pulmonic stenosis.
Symptoms of rheumatic valve disorders:
1. Mitral Valve Disorders
Mitral Stenosis (MS):
- Dyspnea on exertion → due to pulmonary congestion
- Orthopnea and paroxysmal nocturnal dyspnea
- Fatigue and reduced exercise tolerance → due to decreased cardiac output
- Palpitations → often from atrial fibrillation
- Hemoptysis → from pulmonary hypertension
- Right-sided heart failure signs → ankle edema, ascites (in advanced cases)
Mitral Regurgitation (MR):
- Fatigue
- Dyspnea → exertional, progressing to orthopnea
- Palpitations
- Left-sided heart failure signs in chronic MR
2. Aortic Valve Disorders
Aortic Stenosis (AS):
- Exertional dyspnea
- Angina
- Syncope on exertion
- Heart failure symptoms in advanced disease
Aortic Regurgitation (AR):
- Dyspnea and fatigue
- Palpitations
- Wide pulse pressure (bounding pulses)
- Angina (sometimes)
- Heart failure signs in chronic AR
3. Tricuspid & Pulmonic Valve Disorders (Rare)
- Peripheral edema, ascites, hepatomegaly → right-sided heart failure signs
- Fatigue and exercise intolerance
The treatment of Rheumatic Valve Disease
Treatment of Rheumatic Valve Disease (RVD) depends on disease stage, valve involved, severity of dysfunction, and presence of complications. Management is medical, interventional, or surgical.
1. Medical Management
Purpose: Control symptoms, prevent progression, and manage complications.
- Prevention of rheumatic fever recurrence:
- Long-term antibiotics (usually benzathine penicillin G IM every 3–4 weeks)
- Important in patients with a history of rheumatic fever or RVD.
- Heart failure management:
- Diuretics → relieve pulmonary congestion and edema
- ACE inhibitors / ARBs → for ventricular dysfunction
- Beta-blockers / Calcium channel blockers → in atrial fibrillation
- Rate control and anticoagulation:
- Atrial fibrillation common in mitral stenosis/regurgitation
- Warfarin or DOACs to prevent thromboembolism
- Symptom relief:
- Sodium restriction, activity modification, and treatment of infections
2. Interventional Management
- Percutaneous Balloon Mitral Valvotomy (PBMV):
- For severe mitral stenosis with favorable valve morphology
- Minimally invasive alternative to surgery
3. Surgical Management
Indications: Severe valve dysfunction, symptoms despite medical therapy, or complications.
- Valve repair (preferred if feasible)
- Often used in mitral valve disease
- Valve replacement
- Mechanical or bioprosthetic valves
- Indicated in severe stenosis or regurgitation not amenable to repair
- Tricuspid or aortic valve surgery if severe involvement
4. Lifestyle and Supportive Measures
- Avoid strenuous activity if symptomatic
- Prompt treatment of upper respiratory infections
- Regular follow-up with echocardiography