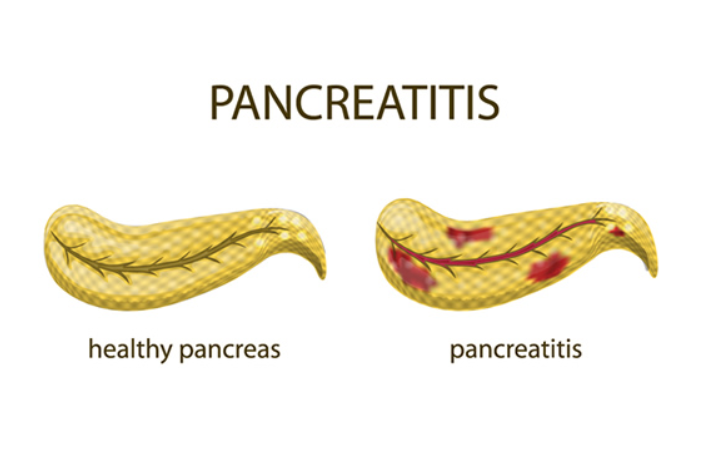
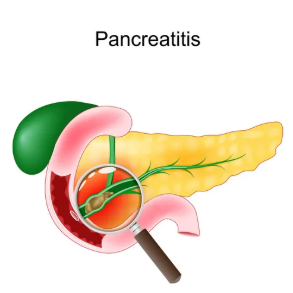
Pancreatitis is the inflammation of the pancreas, an organ located behind the stomach that plays a vital role in digestion and blood sugar regulation.
There are two main types:
- Acute pancreatitis – sudden onset inflammation, often severe but usually reversible with treatment.
- Chronic pancreatitis – long-standing inflammation that leads to permanent damage, scarring, and loss of pancreatic function.
The causes of pancreatitis:
1. Most Common Causes
- Gallstones – Blockage of the pancreatic duct by gallstones can trigger inflammation.
- Alcohol consumption – Chronic heavy drinking is a major cause, especially in adults.
2. Metabolic Causes
- Hypertriglyceridemia – Very high triglyceride levels (>1000 mg/dL)
- Hypercalcemia – Often due to hyperparathyroidism
3. Drug-induced Causes
- Certain medications can trigger pancreatitis, such as:
- Azathioprine
- Valproic acid
- Certain diuretics (e.g., furosemide)
- Some antibiotics (e.g., tetracyclines)
4. Infectious Causes
- Viruses: mumps, coxsackievirus, hepatitis
- Bacterial or parasitic infections (less common)
5. Traumatic or Procedural Causes
- Abdominal trauma
- Post-ERCP (Endoscopic Retrograde Cholangiopancreatography)
6. Genetic and Structural Causes
- Hereditary pancreatitis (mutations in PRSS1, SPINK1 genes)
- Congenital anomalies of the pancreatic ducts
7. Idiopathic
- Sometimes no identifiable cause is found; these are called idiopathic pancreatitis.

The Pancreatitis symptoms:
1. Acute Pancreatitis
- Severe upper abdominal pain – often sudden, may radiate to the back
- Nausea and vomiting
- Abdominal tenderness
- Fever
- Rapid heartbeat (tachycardia)
- Swollen or distended abdomen in severe cases
- Sometimes jaundice if bile duct is involved
2. Chronic Pancreatitis
- Persistent abdominal pain – may be intermittent or constant
- Weight loss – due to malabsorption
- Steatorrhea – oily, foul-smelling stools (fat malabsorption)
- Diabetes mellitus – due to loss of insulin-producing cells
- Nausea and vomiting may also occur
Other signs in severe cases of acute pancreatitis:
- Low blood pressure
- Confusion or lethargy
- Signs of shock (if complicated by necrosis or infection)
The Treatment of pancreatitis
1. Acute Pancreatitis
Main goals: Supportive care, relieve pain, treat underlying cause, prevent complications.
a) Hospital care and supportive measures:
- Fasting (NPO) – allow the pancreas to rest
- IV fluids – to prevent dehydration and maintain blood pressure
- Pain control – usually with opioids
- Nutritional support – enteral feeding if prolonged fasting is needed
b) Treat underlying cause:
- Gallstones – may require ERCP or surgery
- High triglycerides – lipid-lowering therapy
- Medication-induced – stop the offending drug
c) Complication management:
- Infections – antibiotics if infected necrosis occurs
- Surgery – for pancreatic necrosis or abscess
2. Chronic Pancreatitis
Main goals: Manage pain, prevent further damage, replace lost pancreatic function.
a) Lifestyle modifications:
- Avoid alcohol completely
- Low-fat diet
b) Medications:
- Pancreatic enzyme replacement therapy (PERT) – to help digestion
- Insulin – if diabetes develops
- Pain management – analgesics, sometimes nerve blocks
c) Procedures or surgery:
- Drainage of pseudocysts
- Surgery to remove damaged tissue or relieve duct obstruction