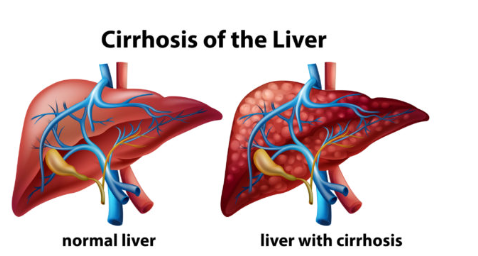
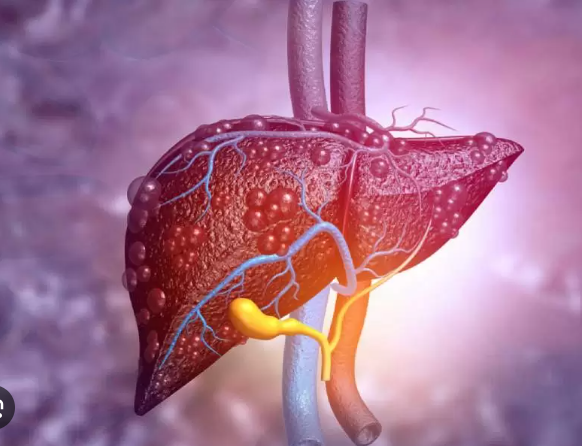
Cirrhosis is a chronic liver disease where healthy liver tissue is replaced by scar tissue (fibrosis). This scarring blocks blood flow through the liver and interferes with its normal functions (detoxification, making proteins, storing energy).
Causes of Cirrhosis:
1. Chronic Alcohol Use (Alcoholic Liver Disease)
- Long-term, heavy drinking damages liver cells.
- Most common cause in many countries.
2. Chronic Viral Hepatitis
- Hepatitis B (HBV) and Hepatitis C (HCV) are major worldwide causes.
- Ongoing inflammation leads to scarring and cirrhosis.
3. Non-Alcoholic Fatty Liver Disease (NAFLD / NASH)
- Linked to obesity, type 2 diabetes, high cholesterol, metabolic syndrome.
- Fat accumulation causes inflammation → scarring.
4. Autoimmune Hepatitis
- Body’s immune system attacks liver cells, causing chronic inflammation and damage.
5. Biliary Diseases (affecting bile ducts)
- Primary Biliary Cholangitis (PBC) – immune-related destruction of bile ducts.
- Primary Sclerosing Cholangitis (PSC) – inflammation/scarring of bile ducts, often linked to inflammatory bowel disease.
6. Genetic & Metabolic Disorders
- Hemochromatosis → excess iron deposits in liver.
- Wilson’s disease → copper buildup in liver.
- Alpha-1 antitrypsin deficiency → abnormal protein damages liver.
7. Long-term Drug or Toxin Exposure
- Certain medications (e.g., methotrexate, isoniazid) or toxins can damage the liver.
the symptoms of cirrhosis:
Early Symptoms (may be mild or absent)
- Fatigue and weakness
- Loss of appetite
- Nausea
- Weight loss
- Mild abdominal discomfort
Advanced Symptoms
- Jaundice → yellowing of the skin and eyes due to bilirubin buildup
- Ascites → fluid accumulation in the abdomen causing swelling
- Peripheral edema → swelling of legs, ankles, and feet
- Easy bruising or bleeding → due to decreased clotting factor production
- Itchy skin (pruritus)
- Spider angiomas → small, spider-like blood vessels visible on the skin
- Red palms (palmar erythema)
Neurological Symptoms
- Hepatic encephalopathy → confusion, memory problems, personality changes, sleep disturbances
- Tremors or a “flapping” hand motion (asterixis)
Gastrointestinal Symptoms
- Loss of appetite and nausea
- Enlarged spleen (splenomegaly)
- Vomiting blood → due to bleeding varices in the esophagus or stomach
- Black, tarry stools → from internal bleeding
the treatment of cirrhosis:
1. Treat the Underlying Cause
- Alcohol-related cirrhosis: Complete abstinence from alcohol.
- Hepatitis B or C: Antiviral medications to reduce liver inflammation.
- Non-alcoholic fatty liver disease (NAFLD/NASH): Weight loss, healthy diet, exercise, managing diabetes or cholesterol.
- Autoimmune hepatitis: Immunosuppressive drugs (e.g., corticosteroids).
- Metabolic/genetic causes: Specific treatments like chelation for Wilson’s disease or phlebotomy for hemochromatosis.
2. Medications to Manage Complications
- Diuretics → reduce fluid buildup (ascites, edema).
- Beta-blockers → prevent bleeding from varices.
- Lactulose or rifaximin → treat hepatic encephalopathy (confusion due to toxin buildup).
- Vitamin and mineral supplements → correct deficiencies (e.g., vitamin K, B-complex, zinc).
3. Lifestyle Modifications
- Avoid alcohol entirely.
- Follow a low-salt diet to reduce fluid retention.
- Maintain a balanced diet with adequate protein (unless advanced liver failure).
- Vaccinations → hepatitis A & B, influenza, pneumococcal vaccines.
4. Procedures / Surgery
- Paracentesis → removing excess abdominal fluid (ascites).
- Endoscopic treatment → banding or sclerotherapy for bleeding varices.
- Liver transplant → for end-stage cirrhosis or liver failure.
5. Monitoring and Supportive Care
- Regular blood tests and imaging to monitor liver function and detect liver cancer early.
- Treat infections promptly, as cirrhosis weakens the immune system.
- Support groups and counseling for lifestyle changes (e.g., alcohol cessation).