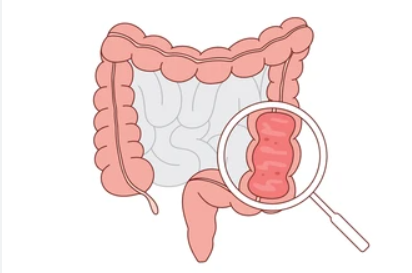
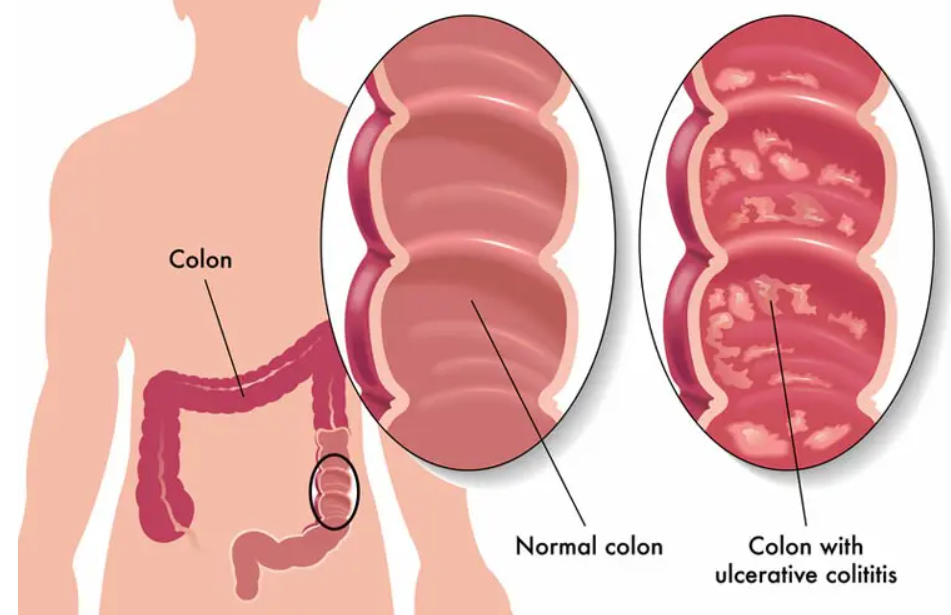
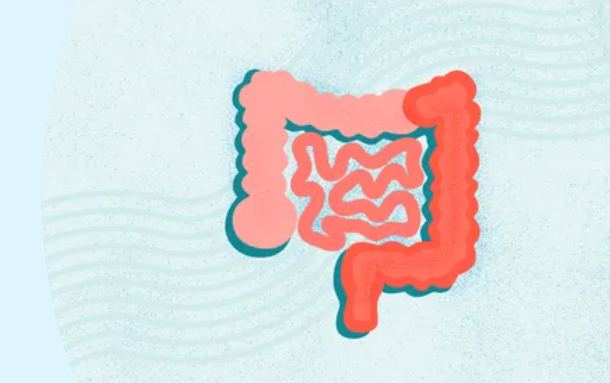
is a type of inflammatory bowel disease (IBD) that causes chronic inflammation and sores (ulcers) in the innermost lining of the large intestine (colon) and rectum. This condition results in symptoms such as abdominal pain, bloody diarrhea, and an urgent need to empty the bowels, though many people experience periods of remission with mild symptoms. It is a lifelong condition, and while there’s no cure, treatments can help manage symptoms, and in severe cases, surgery to remove the colon may be necessary.
The cause of ulcerative colitis (UC):
1. Immune System Dysfunction
- Normally, the immune system attacks harmful bacteria/viruses.
- In UC, the immune system overreacts and attacks the cells of the colon lining.
- This leads to chronic inflammation and ulcer formation.
2. Genetic Factors
- UC tends to run in families → higher risk if a parent or sibling has IBD.
- Several genes (e.g., those related to immune regulation and gut barrier function) are linked to UC.
3. Environmental Triggers
Factors that may trigger or worsen UC include:
- Diet: High-fat, low-fiber diets may contribute (not a direct cause).
- Infections: Certain gut infections may trigger inflammation.
- Smoking: Interestingly, smoking increases Crohn’s risk but seems to reduce UC risk.
- Air pollution / urban living: Linked to higher UC rates.
4. Gut Microbiome Imbalance
- People with UC often have altered gut bacteria (dysbiosis).
- The imbalance may stimulate abnormal immune responses.
5. Other Possible Factors
- Stress and emotional factors don’t cause UC but can worsen flares.
- Some medications (e.g., NSAIDs, certain antibiotics) may trigger flare-ups.
The symptoms of ulcerative colitis (UC):
Common Gastrointestinal Symptoms
- Diarrhea with blood or pus (hallmark symptom)
- Abdominal pain and cramping (often lower left side)
- Urgency to have a bowel movement (tenesmus)
- Frequent bowel movements (sometimes at night)
- Feeling of incomplete emptying after bowel movement
General / Systemic Symptoms
- Fatigue, weakness
- Fever (during flares)
- Loss of appetite, weight loss
- Anemia (from chronic blood loss)
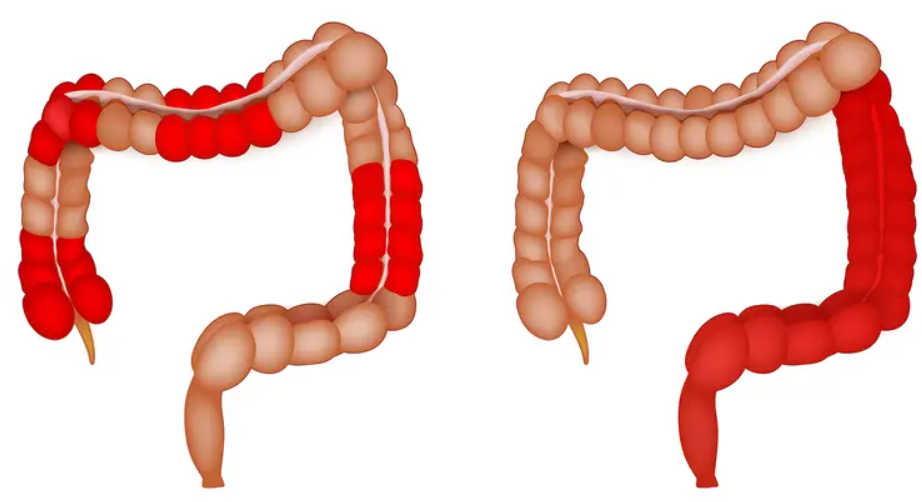
Severity-Based Symptoms
- Mild UC: Fewer than 4 bowel movements/day, small amounts of blood, mild cramping
- Moderate UC: More than 4 bloody stools/day, abdominal pain, mild anemia
- Severe UC: More than 6 bloody stools/day, severe cramps, fever, rapid heartbeat, significant anemia
- Fulminant UC (rare, very severe): Over 10 stools/day, continuous bleeding, toxic megacolon risk
Extra-intestinal Symptoms (outside the gut)
UC can also affect other parts of the body:
- Joints: arthritis, joint pain
- Skin: erythema nodosum (red painful nodules), pyoderma gangrenosum
- Eyes: uveitis (eye pain, redness, blurred vision)
- Liver/bile ducts: primary sclerosing cholangitis (PSC)
Treatment for ulcerative colitis (UC):
1. Medications
a) Aminosalicylates (5-ASA drugs) – First-line for mild to moderate UC
- Examples: Mesalamine, Sulfasalazine, Olsalazine, Balsalazide
- Forms: Oral pills, rectal suppositories, enemas
- Purpose: Reduce inflammation in colon lining
b) Corticosteroids – For flares (short-term use only)
- Examples: Prednisone, Budesonide, Hydrocortisone enemas
- Use: Control moderate–severe flares when 5-ASA isn’t enough
- Limitation: Not for long-term use due to side effects (weight gain, diabetes, osteoporosis)
c) Immunomodulators – For steroid-dependent/refractory cases
- Examples: Azathioprine, 6-Mercaptopurine (6-MP), Methotrexate
- Purpose: Suppress abnormal immune response
- Slow onset: May take weeks–months to work
d) Biologic Therapies – For moderate to severe UC
- Anti-TNF agents: Infliximab, Adalimumab, Golimumab
- Anti-integrins: Vedolizumab (gut-specific)
- Anti-interleukin: Ustekinumab
- JAK inhibitors (oral small molecule): Tofacitinib, Upadacitinib
- Purpose: Target specific immune pathways to control inflammation
e) Other Medications
- Antibiotics → for infections or complications
- Antidiarrheal (loperamide) → only in mild cases, not during severe flares
- Iron supplements → for anemia
- Pain management → acetaminophen (avoid NSAIDs as they may worsen UC)
2. Surgery
- Colectomy (removal of colon/rectum) is curative for UC
- Indications:
- Severe disease not responding to meds
- Complications (toxic megacolon, perforation, massive bleeding)
- High risk of colon cancer
- Common surgery: Proctocolectomy with ileal pouch–anal anastomosis (IPAA) → allows bowel movements without permanent ostomy
3. Lifestyle & Supportive Care
- Diet: No single “UC diet,” but patients may benefit from:
- Low-residue diet during flares (less fiber, reduces bowel movements)
- Avoiding trigger foods (spicy, fatty, caffeine, alcohol, lactose if intolerant)
- Hydration: Prevent dehydration from diarrhea
- Stress management: Stress can worsen symptoms (but doesn’t cause UC)
- Regular follow-up colonoscopies: Cancer risk increases with disease duration and severity